Should I Stay or Should I Go (to the Hospital in July)?
This article was original published on Medium.
If you’re going to get sick, and I mean really sick, enough to land you in the hospital, think about this: July 1 is around the corner, and on that day, medical students fresh out of school start their clinical rotations at hospitals and outpatient clinics, first year residents are promoted from “intern” to second year resident, and at teaching hospitals all across the U.S., everyone in training is given responsibilities they’ve never had before and feel unprepared to handle. And there you are, sick as a dog, in a cold exam room, trying to cover your butt because the hospital gown they gave you has only one tie.
There’s some evidence that death rates go up and efficiency goes down at teaching hospitals in July, but no firm conclusions about how serious this is.
For over two decades, I worked in Graduate Medical Education, observing the life cycle of residency and fellowship play itself out year after year as we welcomed new trainees, and watched them rise through the ranks, gradually acquiring new skills, competencies, and confidence. Imposter syndrome is rife throughout training, and worst in the first months of intern year. Some people go through life “faking it” but for physicians, who are generally Type-A personalities, feeling like a fraud is especially painful.
So, while you’re shivering on your narrow cot, if your doctor’s ID badge says RESIDENT, imagine how scared they are. Just weeks after medical school graduation and the feeling of accomplishment that accompanies it, interns meet their colleagues, compare notes on where they went to school, and find their place, sure that everyone else knows more than they do, and terrified of showing their ignorance. Twelve rotations later, interns rise to become second year residents, and take on new responsibilities. Now it’s their turn to teach the newly arrived interns, and the residency education lifecycle begins again.
Medical training is a team sport. The job of every resident is to learn, and there’s always someone more senior, more experienced than you to help with making decisions. As the director of an onsite counseling office dedicated to supporting the 1,500 doctors-in-training at a large teaching hospital in Seattle, I heard about imposter syndrome all the time. Another common attitude among doctors is the sense that EVERYTHING DEPENDS ON YOU, as if the weight of the world is carried on your shoulders alone. My job was to support the residents, help them gain perspective, and strike a balance between “I’m responsible for everything,” and “how can you expect me to know everything, I’m here to learn!”
One early July morning, a second year OB-GYN resident came to my office and opened with “I killed a baby last night.” She believed she was responsible for a tragic outcome, as if none of her other team members had been in the room with her. I asked her to take me back to the previous night, tell me what happened. Here’s what she told me:
At 11 pm, Joan was pedaling furiously, racing to the hospital. The sun had set only 2 hours ago, leaving wisps of light reflected in the clouds. The crisp summer-night air invigorated her. Navigating the steep, dark Seattle streets, she mentally practiced a new stitch. Left over right, right over left, she reviewed each surgical step, until it began to feel like muscle memory. Only last week, Joan was in the final days of intern year. When it began a year ago, fresh out of medical school, she and the other first-year OB-GYN residents were relegated much of the time to scut work: menial, non-patient-care tasks assigned to medical students and interns, those lowest on the rungs of medical hierarchy. On July 1, the clock reset, and she rose to second-year status. No longer an observer, she would now be actively involved in deliveries and get to do her first Caesarian Section.
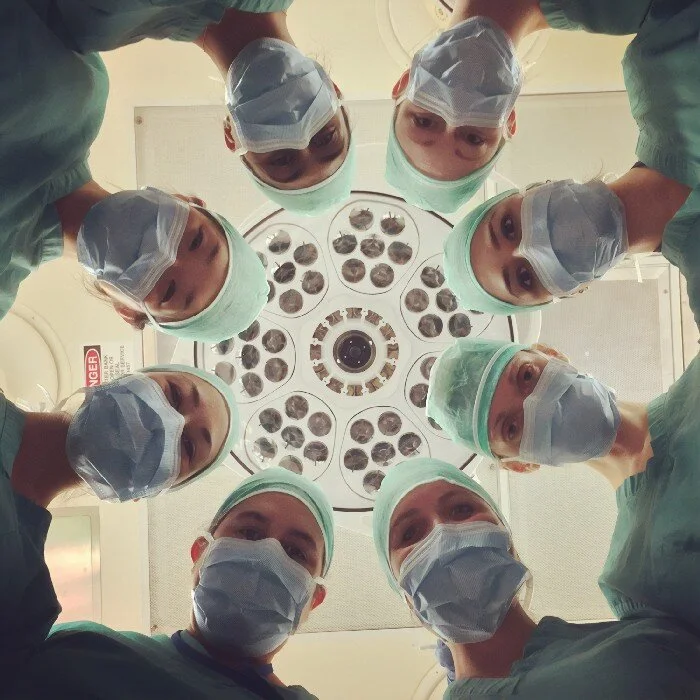
Removing her helmet, Joan’s pager exploded with multiple messages. It was 11:30 pm. A laboring mom was arriving momentarily by ambulance. Locking her bike, she heard the siren and saw the emergency room’s driveway bathed in red, blinking light. Joan rushed to the L&D suites, quickly stripping out of street clothes and donning sterile scrubs. Shoving her sweat-stained biking gear into a locker, Joan discreetly whiffed her underarms. “Not too pungent,” she told herself. “It’s showtime — bring it on!” Preparing to accept the new patient, each member of his team had a clear role. Third- and fourth-year residents, the maternal-fetal medicine (MFM) fellow, plus an Attending pediatric physician that all of them revered, filed one by one into the surgery suite. “Wow. This is a dream team. How cool is that?” Joan was stoked. She was reassured. The one thing she wasn’t was scared. With expertise like this, what could go wrong?
As the laboring mom was wheeled into the L&D suite, Joan saw the crimson stains on the bedding. Glancing up, she noted the time: midnight. What had taken them so long? The team that accompanied the mom from the regional hospital peeled away, handing over care to the trauma center’s experts. The mother, bleeding profusely, required an emergency C-section. Joan had witnessed dozens of C -sections before, but never under this kind of pressure. The MFM fellow directed the surgical nurse to call the Attending’s partners for more pediatric support, and for the Chair of her department to come in as backup. The third-year resident was dispatched to retrieve four bags of blood for the mother. The atmosphere was controlled chaos as eight different people crowded around the patient. Joan’s place in the icy room was front and center. Her heart clanged loudly as lines of sweat trickled down her back, tingling her spine. At 12:30 am, the MFM fellow began the Caesarian. Within minutes, Joan was cradling the baby’s head. Giving the senior resident a nod, she watched her reach under the baby’s bottom to lift a tiny boy out of its mother’s uterus, the umbilical cord wrapped tightly around his neck. Working deftly to separate the boy from his mother, Joan saw the baby’s color, already dark, turn a ghastly blue. Her nimble fingers worked furiously to free the child from the grasp of the cord and pass him on to the pediatric team. The Attending pediatrician, realizing the dimming odds of success, glowered at the baby, as if willing him to live. “Breathe! Breathe, God-damn it!” she cursed. Half a dozen hands reached out to the newborn, each performing a different task in a desperate group attempt to keep him alive. The Attending shook her head morosely, and her eyes darted around the room, searching for someone, something to change the outcome. The child could not be saved. The mother was hemorrhaging. More and more blood was transfused — after eight units, she finally stabilized. At 1:00 am they began wrapping up. One dead baby. One live mother. Eight exhausted team members, all of them morose. It had nothing to do with the time of year. It was just rotten, bad luck.
Joan’s shift was just beginning. She had nine more hours to go before she could sign out at noon.
When her senior resident told her to get breakfast at 9:00 am, Joan walked over to the cafeteria to eat and to steady her nerves. She knew the counseling office was right around the corner. Sitting alone, she gulped down her eggs and hash browns, refilled her coffee cup, then exited the cafeteria from a side door and cautiously peered down the hall to see if my office door was open. I looked up to see a tall woman, ruffling her free hand through curly hair. Meeting my gaze, she asked, “Are you available to talk? I know you aren’t expecting me, and I’m only free for a few minutes, but….” I closed the door behind her and encouraged her to take a seat. “What’s going on?” I asked. “Something must be really bothering you.” With a shaky voice, Joan began, “I need to talk with someone. I killed a baby last night.”
I had to help Joan see that she had been part of a team so she could work through her guilt. A baby had died, despite many dedicated people working to prevent this outcome. Yet this tragedy wasn’t caused by her neglect or lack of knowledge. Bad things sometimes happen. Joan needed to accept this and stop blaming herself, needed to reframe her thinking and begin to believe, “A baby died, and all of us feel awful. We all need to learn from this, and we will. Our team will participate in a full review of what happened, and some protocols may change if we learn anything was missed. We did the best we could. It wasn’t my fault.” Until she accomplishes this, Joan’s ability to act decisively will be compromised as every step she makes is second-guessed. Doctors who are involved in medical errors suffer consequences in both their personal and professional lives, and at worst, are at risk for self-harm.
If it’s just your luck to land in a hospital as the clock is resetting in July, remember this: a teaching hospital is still a great place to get medical treatment, because whoever takes care of you is part of a much deeper bench, with knowledge of the latest, most up-to-date, evidence-based information. You’ll be in good hands, even if your butt is freezing in that flimsy hospital gown.